California is experiencing a sharp resurgence of COVID-19 in July–August 2025, with cases more than doubling statewide compared to early summer. According to the Los Angeles Times (Sept 3, 2025), public health officials are urging residents to mask up again as emergency department visits and positivity rates climb.
The latest CDC modeling confirms this rise: Rt (the effective reproduction number) is now above 1.2 in many counties, signaling epidemic growth. In simple terms, every infected individual is now spreading the virus to more than one other person, a clear indicator of sustained transmission.
For residents in South Bay communities, many are once again turning to Urgent Care in Torrance for timely testing, treatment, and peace of mind. These centers remain a frontline resource for those who need quick medical support without the long wait times of hospitals.
This summer surge has reignited conversations around public safety, testing, vaccination, and preparedness. Below, we dive deep into epidemic trends, healthcare responses, and what Californians can do to stay safe
Table of Contents
Toggle2. Epidemic Trends and Rt Analysis: What the Data Shows
The Rt value (reproductive number) is a critical metric in understanding epidemic growth. It measures how quickly the virus is spreading. When Rt > 1, the outbreak is expanding; when Rt < 1, cases are declining.
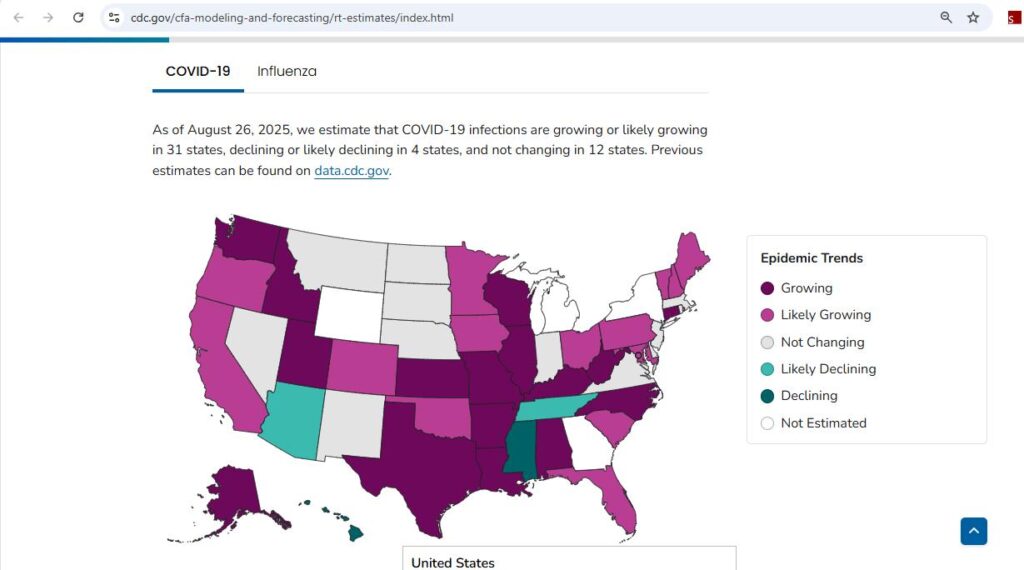
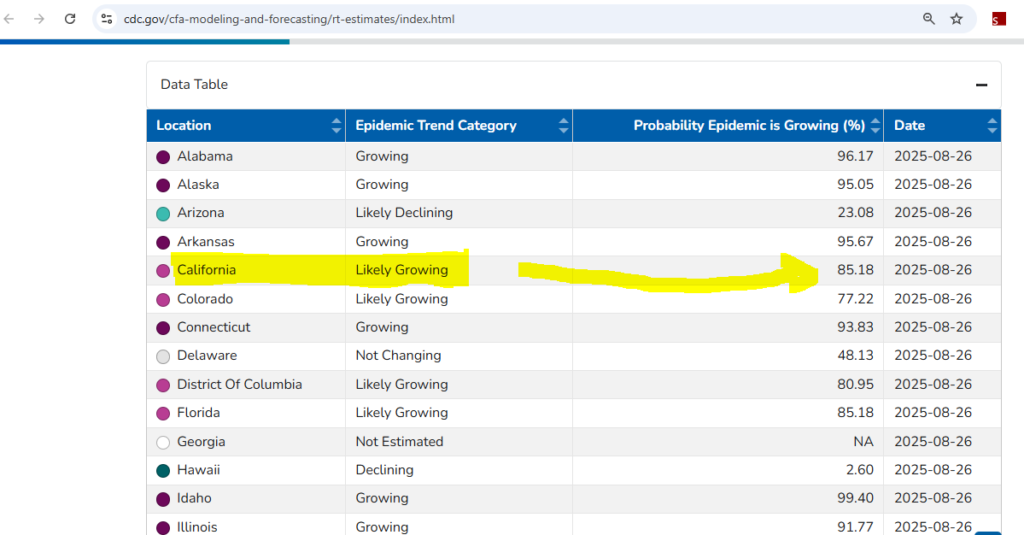
According to CDC Rt estimates (Aug 26, 2025):
- COVID-19 infections are growing in 31 U.S. states, including California.
- In 4 states, infections are declining.
- In 12 states, infections are stable.
California’s Rt has remained above 1.2 for weeks, highlighting sustained epidemic expansion. Emergency department visits related to COVID-19 have also risen by more than 40% since July, underscoring the pressure on the healthcare system.
It’s essential to note that Rt alone does not accurately reflect disease burden. It must be viewed alongside hospital admissions, ICU occupancy, and ED visit percentages. California currently shows a significant ED burden, making this surge one of the most concerning since the winter wave of 2022–23.
3. Why California Is Seeing a Summer Surge in 2025
Several factors contribute to the rise in infections this summer:
- Variants in circulation: New Omicron subvariants (e.g., KP.3 and KP.4) are highly transmissible, bypassing partial immunity from older infections.
- Declining immunity: Many residents have not received a recent booster, leaving them vulnerable.
- Indoor gatherings: High summer heat drove more people indoors, increasing exposure risk.
- Travel patterns: Summer tourism and domestic travel created more opportunities for transmission.
- Mask fatigue: Relaxed precautions have reduced public masking and distancing.
This convergence of factors explains why California’s summer has turned into what experts are calling a “Stratus Summer”, a wave that feels familiar, but carries unique challenges in 2025
4. Public Health Guidance: Masks, Vaccines, and Boosters
Health officials in California, including those in Los Angeles County, are urging residents to mask up indoors in crowded settings once again.
Key recommendations:
- Masks: High-quality respirators (N95/KN95) are most effective.
- Vaccination: Updated 2025 boosters target circulating Omicron subvariants. The CDC recommends boosters for:
- Adults over 50
- Immunocompromised individuals
- People with chronic health conditions
- Testing: Get tested if you experience symptoms or before visiting high-risk individuals.
- Stay home if sick: Even mild symptoms can spread the virus.
California’s health system has learned from past surges, testing and vaccination access are widely available, but public compliance is the variable that makes or breaks containment. It is quite natural to panic during such situations, but that’s not the solution. You need to get started by checking with your nearby urgent care if you or your family members may need some COVID-19 vaccinations.
Sometimes during such surges, the urgent care tends to be busy with vaccinations and other mild symptoms; however, residents in Torrance can still check in for Minor Injuries and other emergencies that need attention.
5. COVID Testing in California: Options, Access, and Urgent Care Support
Testing remains the backbone of outbreak control. Californians have access to:
- At-home antigen tests (widely available at pharmacies).
- PCR tests at urgent care clinics and hospitals.
- Rapid same-day testing at specialized centers.
At clinics like Life Saver Urgent Care in Torrance, patients can access same-day PCR results, crucial for travel, work clearance, or school safety. (See also: Minor Injuries with On-Site Rehabilitation in Torrance blog for how urgent care services extend beyond COVID).
Testing trends in California:
- Demand for PCR tests has risen 70% since July 2025.
- Some counties have reopened community testing kiosks.
- Federal programs continue to provide free test kits for eligible households.
Reliable testing ensures early isolation, treatment, and reduced community spread.
6. Impact on Workplaces, Schools, and Communities
The surge has ripple effects across daily life in California.
Workplaces:
- Employers are reinstating hybrid policies to minimize in-office exposure.
- Some industries, especially healthcare and hospitality, are mandating masking indoors.
Schools:
- School districts are distributing free test kits.
- Policies allow flexible attendance for students testing positive but not severely ill.
- Mask mandates have not yet returned, but officials are urging voluntary compliance.
Communities:
- Local events and gatherings are seeing reduced attendance.
- Some festivals and concerts have added on-site rapid testing booths.
While not as disruptive as early pandemic years, these adjustments highlight how COVID-19 continues to reshape social and economic activity.
7. Travel in 2025: Testing, Certificates, and Safety Rules
- Domestic Travel: No federal test requirements but testing before visiting vulnerable relatives is advised.
- International Travel: Some destinations (e.g., parts of Asia and South America) still require negative PCR certificates.
- Airports: LAX has reinstated mask advisories, though not mandates.
- Cruises: Require either proof of vaccination or recent negative tests.
8. Coping with Long COVID and Post-Surge Recovery
While the immediate spike in cases dominates headlines, the long-term effects of COVID-19 remain one of the most pressing public health concerns. Commonly referred to as “Long COVID” or post-acute sequelae of SARS-CoV-2 infection (PASC), this condition can last for months or even years after the initial infection.
Most reported symptoms include:
- Brain fog — difficulty concentrating, poor memory, or confusion.
- Chronic fatigue — extreme tiredness that isn’t relieved by rest.
- Shortness of breath — lingering respiratory difficulties.
- Anxiety and depression — linked to both neurological impacts and the stress of prolonged illness.
- Sleep disturbances and chest pain — noted in clinical follow-ups across California.
California’s Response to Long COVID
Healthcare providers have responded by establishing specialized post-COVID care centers.
These clinics offer:
- Pulmonary rehabilitation for patients with lung damage or persistent breathing issues.
- Cognitive therapy programs aimed at restoring memory and focus.
- Nutritional counseling to help patients rebuild strength.
- Mental health support groups to address anxiety and depression associated with Long COVID.
A 2025 CDC report estimates that 10–15% of all infected patients will experience Long COVID. For California, where millions have already been infected, this translates into hundreds of thousands of residents needing ongoing care. Economists warn this could contribute to significant lost workdays and rising healthcare costs, especially among working-age adults.
Key takeaway: If symptoms persist beyond four weeks post-infection, residents should seek medical evaluation immediately. Early treatment interventions have been shown to improve long-term recovery outcomes.
9. Community and Policy Response in California
California has long been at the forefront of pandemic management, and this summer surge has prompted a renewed wave of preventive actions.
Statewide Measures Implemented:
- Stockpiling N95 masks for emergency distribution through county health departments.
- Expanding telehealth services, ensuring patients with mild to moderate illness can access physicians without overwhelming emergency rooms.
- Offering free booster clinics in community centers, schools, and mobile vans for residents in underserved areas.
- Partnering with local nonprofits and faith-based groups to boost outreach among vulnerable populations, including low-income and immigrant communities.
County-Level Guidance
- Los Angeles and Orange counties have issued advisories, encouraging indoor masking but stopping short of mandates.
- Counties are focusing on personal responsibility, urging residents to make informed decisions rather than enforcing blanket restrictions.
Comparison to Other States
Unlike some states where the response has been more reactive, California’s preventive approach aims to flatten the curve before hospitalizations peak.
This strategy reflects lessons learned from earlier surges in 2020–2022, where delayed action led to overburdened hospitals. In comparison to other states in the United States, California is in the growing stage in terms of the surge.
10. Staying Prepared: Practical Safety Tips for Residents
Every Californian has a role to play in limiting transmission. While state and county policies provide a safety net, personal preparedness remains the most powerful tool.
At-Home Preparedness Checklist:
- Keep at-home antigen tests readily available for quick screening.
- Maintain a stock of high-quality masks (N95 or KN95).
- Have a thermometer and pulse oximeter at home to monitor symptoms.

Day-to-Day Precautions:
- Wear an N95 indoors in crowded spaces like grocery stores, gyms, and public transit.
- Stay current on boosters, especially if you’re over 50 or have chronic conditions.
- Leverage telehealth for mild illness, it saves time and reduces clinic crowding.
- Ensure good ventilation indoors by opening windows or using HEPA filters.
- Test before visiting vulnerable family members, like grandparents or immunocompromised relatives.
Staying Informed
- Regularly check the CDC COVID Data Tracker for national updates.
- Follow California Department of Public Health dashboards for county-level advisories.
- Sign up for local health alerts to get real-time updates on vaccination drives and testing locations.
Bottom line: Preparedness reduces anxiety, prevents panic, and empowers Californians to take control of their health during uncertain times.
11. Comparing COVID with Flu and RSV in 2025
As fall approaches, health officials warn of a possible “tripledemic”, the convergence of COVID-19, seasonal influenza, and RSV (respiratory syncytial virus).
Flu Outlook 2025
- Early indicators from the Southern Hemisphere suggest that 2025 could bring a more severe flu season than usual.
- Vaccination remains the strongest defense, with updated flu shots available at clinics statewide.
RSV in Focus
- RSV primarily affects infants, toddlers, and older adults, often leading to hospitalization.
- The recent approval of RSV vaccines for seniors and preventive antibody treatments for children offers new protection options in 2025.
COVID-19 vs Flu and RSV
- COVID-19 continues to show higher hospitalization and mortality rates compared to flu and RSV.
- Unlike flu, COVID can cause long-term complications such as Long COVID, adding a layer of public health concern.
- RSV poses a serious pediatric risk, but COVID’s impact remains broader across all age groups.
Why a Combined Approach Matters
Health experts recommend a multi-layered prevention strategy:
- Get your COVID booster (updated for new Omicron subvariants).
- Receive your flu shot as early as September.
- Eligible groups (seniors, children) should consider RSV vaccination.
By combining these preventive steps, Californians can reduce strain on hospitals and protect their families from multiple respiratory threats this fall.
12. The Road Ahead: What Californians Can Expect in Fall and Winter
If current Rt values persist, California may see:
- Increased hospitalizations by late fall.
- Renewed mask mandates in schools if absences rise.
- Expanded testing kiosks and vaccine drives.
However, experts stress that community action can flatten the curve. Early adoption of masking and vaccination could prevent a repeat of the harsh winter waves seen in prior years.
13. Resilience in the Face of Uncertainty
The Stratus Summer surge of 2025 is a reminder that COVID-19 remains unpredictable. While less disruptive than in 2020, the virus continues to test California’s preparedness and resilience. By combining vigilance with vaccination, testing, and responsible choices, Californians can safeguard both personal health and community well-being.
FAQ’s
Due to new variants, waning immunity, indoor gatherings, and relaxed precautions.
It means infections are spreading faster than they are being controlled — signaling epidemic growth.
Yes, especially in crowded indoor spaces. N95/KN95 masks offer the best protection.
Urgent care centers like Life Saver Urgent Care offer same-day PCR testing.
Yes. Roughly 10–15% of patients experience long-term symptoms, requiring medical care.
COVID carries higher risks of hospitalization, though flu and RSV remain serious threats.
Stay vaccinated, stock at-home tests, mask in crowded settings, and follow county health updates.



